Pathophysiology of Lung Cancer
Pathophysiology of Lung Cancer
Estimated Read Time: 8 minutes
Lung cancer pathophysiology refers to the biological and cellular changes in the lungs that lead to or result from cancer. These changes begin within lung tissue and can eventually affect other areas of the body as the disease progresses.
Types of Lung Cancer
Lung cancer is categorized into two main types:
-
Non-small cell lung cancer (NSCLC) – Accounts for 80–85% of cases.
-
Small cell lung cancer (SCLC) – Makes up 10–15% of cases and is often linked to smoking.
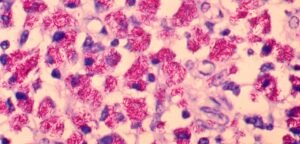
Subtypes of Non-Small Cell Lung Cancer
-
Adenocarcinoma: Arises in mucus-producing cells.
-
Squamous cell carcinoma: Begins in the flat cells lining the airways.
-
Large cell carcinoma: Identified by large, abnormal-looking cells, usually found in the outer regions of the lungs.
Small Cell Lung Cancer (SCLC)
Also referred to as oat cell carcinoma, this aggressive cancer type grows quickly and is strongly correlated with tobacco use.
What Does Pathophysiology Mean?
Pathophysiology is the study of the physical and biological abnormalities that develop as part of a disease process. The term originates from Greek: pathos (suffering), physis (nature), and logos (study).
Leading Causes of Lung Cancer
-
Smoking: Tobacco use is the primary risk factor, responsible for about 80% of lung cancer deaths. Small cell lung cancer is especially tied to smoking history.
-
Other Risk Factors:
-
Secondhand smoke
-
Radon gas exposure
-
Air pollution
-
Asbestos exposure
-
Occupational hazards (e.g., diesel fumes, chemical agents)
-
Firsthand vs. Secondhand Smoke Exposure
People exposed to secondhand smoke also face significant risk. Lung cancers in non-smokers often have different cellular and genetic characteristics compared to those in smokers.
Genetic Factors in Lung Cancer
-
Inherited Genetic Mutations:
Although inherited mutations rarely cause cancer directly, they can increase susceptibility. For example:-
Mutations on chromosome 6 can heighten risk, even in non-smokers.
-
Some people may lack the enzymes to break down harmful substances in tobacco or repair damaged DNA effectively.
-
-
Acquired Gene Mutations:
Most mutations involved in lung cancer occur over a lifetime due to environmental exposure. These DNA changes affect how lung cells grow and divide. -
Important Cancer-Linked Genes:
-
Oncogenes: Promote cell growth and division.
-
Tumor suppressor genes: Regulate cell death and growth control.
-
-
Common Gene Mutations Linked to Lung Cancer:
-
RB1 – SCLC
-
p16 – NSCLC
-
K-RAS – NSCLC
-
TP53 – Found in both SCLC and NSCLC
-
-
Chromosomal Changes and Translocations:
Certain chromosomal abnormalities and gene translocations are linked to lung cancer:-
ALK gene translocation – NSCLC
-
Changes on chromosome 3 – Associated with both SCLC and NSCLC
-
A 2020 meta-analysis found no significant association between BRCA1/BRCA2 mutations and lung cancer.
-
Environmental and Occupational Exposures
-
Tobacco Products:
Cigar and pipe smoke are nearly as harmful as cigarette smoke in terms of cancer risk. Secondhand smoke alone causes around 7,000 lung cancer deaths annually in the U.S. -
Radon Gas:
An invisible, odorless radioactive gas, radon is the second most common cause of lung cancer in non-smokers. It typically enters homes through cracks in the foundation.
One in 15 U.S. homes may have unsafe radon levels. Home test kits are widely available to check radon concentration. -
Asbestos Exposure:
Often found in workplaces such as shipyards, mines, textile plants, and construction sites, asbestos significantly raises lung cancer risk—especially for smokers.
Asbestos exposure is also a major cause of mesothelioma, a rare cancer of the lung lining (pleura). -
Additional Workplace Carcinogens:
Exposure to the following substances can elevate lung cancer risk:-
Uranium
-
Arsenic
-
Beryllium
-
Cadmium
-
Silica
-
Nickel compounds
-
Chromium compounds
-
Mustard gas
-
Diesel exhaust
-
Coal products
-
Chloromethyl ethers
-
Vinyl chloride
-
-
Radiation Exposure:
People who have received radiation therapy to the chest—for conditions like Hodgkin lymphoma or breast cancer—may be at higher risk of developing lung cancer, especially if they smoke. -
Air Pollution:
Outdoor air pollution is estimated to cause about 5% of global lung cancer deaths. While it’s hard to control personal exposure, it remains a significant environmental concern.
Family History and Genetic Predisposition
Having a close relative with lung cancer may increase your personal risk. If you have a family history, consult your healthcare provider to assess your risk and explore early screening options.
Emerging Risk Factors
Some substances are being studied for possible links to lung cancer, although conclusive evidence is not yet available. These include:
-
Marijuana smoke
-
E-cigarettes
-
Talc and talcum powder
Symptoms of Lung Cancer
Lung cancer often doesn’t cause noticeable symptoms in its early stages. When symptoms do appear, it may mean the cancer has spread. Common symptoms include:
-
Persistent cough
-
Chest pain
-
Difficulty breathing
-
Unexplained weight loss
-
Coughing up blood
Frequently Asked Questions
-
What Is the Pathophysiology of Lung Cancer?
It involves structural and functional changes in lung cells that promote abnormal growth and malignancy, often triggered by genetic mutations or environmental exposures.
Expert Tips
-
Maintain a smoke-free environment to reduce both firsthand and secondhand exposure.
-
Test your home for radon, especially if you live in high-risk areas.
-
Wear protective gear if you work in environments with known carcinogens.