Osteomalacia and Bone Pain
Understanding Osteomalacia and Bone Pain
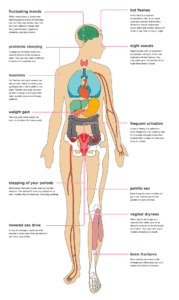
Osteomalacia, a condition that softens the bones, leads to symptoms such as bone pain, muscle weakness, difficulty walking, and an increased risk of fractures. It is typically caused by a deficiency in vitamin D, which hinders the body’s ability to absorb calcium, a vital mineral for bone health. In children, osteomalacia can impair bone development and is often referred to as rickets. This condition is more common among pregnant individuals, those with darker skin, older adults, and people with limited sun exposure.
Additionally, specific medications and conditions like lactose intolerance and allergies can reduce the body’s ability to absorb calcium, further exacerbating the risk of osteomalacia. This article covers the causes, symptoms, diagnosis, and treatment of osteomalacia, with a focus on prevention through dietary sources of nutrients and supplements.
Symptoms of Osteomalacia
While osteomalacia may not always present noticeable symptoms, some individuals experience the following:
-
Bone Pain: This is a common complaint, often affecting the lower back, hips, and legs.
-
Muscle Weakness: This is often associated with difficulty in movement.
-
Joint Issues: Swelling or discomfort in the joints can occur.
-
Loss of Height: A gradual reduction in height may be observed.
-
Increased Fracture Risk: Osteomalacia weakens the bones, making them more prone to fractures from even minor falls.
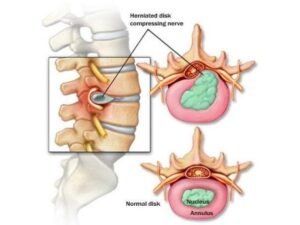
Individuals with advanced osteomalacia may experience deformities in the skeleton, such as a severely hunched back (kyphosis). A “waddling” gait, known as bilateral paid Trendelenburg gait, is another symptom. Difficulty rising from a seated position or climbing stairs is also common, with pain intensifying when weight is placed on the affected bones.
Causes of Osteomalacia
Osteomalacia results from a disruption in the process of bone mineralization. During this process, minerals like calcium and phosphate are supposed to harden the bones, ensuring they remain strong. However, in osteomalacia, these minerals fail to properly incorporate into the bone matrix, resulting in soft, weakened bones. Vitamin D plays a crucial role in this process, and a deficiency can prevent the bones from properly mineralizing.
Factors contributing to osteomalacia include:
-
Vitamin D Deficiency: Insufficient vitamin D intake, especially in vegetarian diets, can be a major cause.
-
Limited Sun Exposure: The body needs sunlight to produce vitamin D, and a lack of exposure can lead to deficiency.
-
Chronic Illnesses: Conditions like liver disease, certain cancers, and digestive surgeries (such as gastric bypass) can interfere with calcium absorption.
-
Medications: Certain medications, such as anticonvulsants, can affect vitamin D metabolism.
Other diseases such as celiac disease, Paget’s disease, and hyperparathyroidism can also contribute to osteomalacia. A deficiency in phosphate, a mineral essential for bone hardening, is another cause, which can be due to rare genetic disorders or cancers that lower phosphate levels.
Osteomalacia vs. Osteoporosis
Though osteomalacia and osteoporosis both affect the bones, they are distinct conditions. Osteomalacia softens the bones due to insufficient mineralization, whereas osteoporosis causes bones to become fragile and brittle due to the breakdown of bone tissue and inadequate bone formation. Osteomalacia is primarily linked to mineral deficiencies, while osteoporosis involves a reduction in bone mass and strength.
Diagnosing Osteomalacia
Diagnosis begins with a thorough medical history and physical examination. Osteomalacia can often be overlooked, particularly in its early stages, as its symptoms can resemble those of other conditions, such as polymyalgia rheumatica or fibromyalgia. Lab tests are essential for diagnosis, with common tests including:
-
Blood Tests: These may reveal low vitamin D levels, high alkaline phosphatase, and abnormal levels of calcium and phosphate.
-
Urine Tests: These tests can help assess calcium and phosphate levels.
-
X-rays and Imaging: If necessary, imaging tests like X-rays can help identify bone changes.
-
Bone Biopsy: In rare cases, a biopsy may be performed under anesthesia, though it is not typically required.
Treatment of Osteomalacia
The treatment of osteomalacia depends on its underlying cause. For vitamin D deficiency-related osteomalacia, high-dose vitamin D supplementation is the primary treatment, usually starting with a large dose for a few weeks or months. Calcium supplements may also be recommended. Monitoring through regular blood tests ensures that the treatment is effective and allows for adjustments as needed. In cases where the osteomalacia is caused by another medical condition, addressing that condition is essential for managing the disorder.
Preventing Osteomalacia
Prevention largely focuses on maintaining adequate levels of vitamin D and calcium through dietary sources and supplements. Foods rich in vitamin D, such as fatty fish, fortified milk, and egg yolks, can help, along with regular sun exposure. For those with limited sun exposure or dietary restrictions, supplements may be necessary to ensure proper bone health.
Key Takeaways
-
Osteomalacia results from a lack of vitamin D, leading to soft and weakened bones.
-
The condition causes symptoms such as bone pain, muscle weakness, joint issues, and an increased risk of fractures.
-
Osteomalacia can be treated with vitamin D supplements and calcium, depending on the underlying cause.
-
Prevention involves ensuring adequate vitamin D and calcium intake through diet, sun exposure, and supplements when necessary.
By understanding the causes and symptoms of osteomalacia, individuals can take proactive steps to manage and prevent this condition, ensuring better bone health and overall well-being.