Osteoarthritis vs. Rheumatoid Arthritis_ Key Differences
Osteoarthritis vs. Rheumatoid Arthritis: Key Differences Explained
Introduction: Understanding the Basics of OA and RA
Osteoarthritis (OA) and Rheumatoid arthritis (RA) are two of the most common forms of arthritis, but they differ significantly in their causes, symptoms, and treatments. OA, affecting over 32 million people in the U.S., is the most prevalent type, while RA, an autoimmune condition, impacts around 1.5 million Americans. Although both conditions fall under the arthritis umbrella, they present different challenges and require unique approaches to management. In this article, we’ll explore the primary differences between OA and RA, their causes, risk factors, and treatment options.
Osteoarthritis vs. Rheumatoid Arthritis: A Closer Look
Osteoarthritis (OA): A Degenerative Joint Condition
Osteoarthritis is commonly referred to as “wear and tear” arthritis. It occurs when the cartilage that cushions the joints breaks down over time, leading to the bones rubbing together. This degeneration results in pain, swelling, and reduced joint mobility. OA typically affects one joint at a time, and its severity increases with age. The joints most commonly impacted by OA include the knees, hips, spine, and hands.
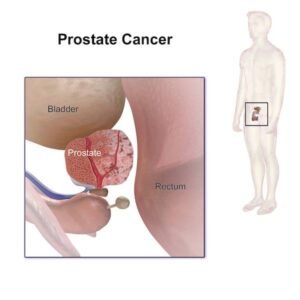
Rheumatoid Arthritis (RA): An Autoimmune Disorder
Unlike OA, Rheumatoid arthritis is an autoimmune condition where the body’s immune system mistakenly attacks its own tissues, specifically the synovium (the lining of the joints). This causes inflammation that can affect multiple joints, and in some cases, other organs in the body. RA most often begins between the ages of 30 and 60, and it is more prevalent in women than men. The disease commonly affects joints such as the wrists, knees, and hands.
Key Differences Between OA and RA
| Osteoarthritis (OA) | Rheumatoid Arthritis (RA) |
|---|---|
| Degenerative | Autoimmune |
| Primarily affects cartilage | Affects joint lining (synovium) |
| Typically affects one joint at a time | Affects multiple joints, often symmetrically |
| More common in people over 65 | Most common between ages 30-60 |
| Gender-neutral | More common in assigned females |
| Risk factors: age, joint injury, overuse, obesity | Risk factors: genetics, smoking, diet, environmental exposure |
Symptoms of Osteoarthritis and Rheumatoid Arthritis
While OA and RA share some symptoms, they also have distinct characteristics. For instance, both conditions cause joint pain and stiffness, but the duration and intensity of these symptoms vary.
Osteoarthritis Symptoms:
-
Joint pain, especially after repetitive motion or physical activity
-
Morning stiffness lasting less than 30 minutes
-
Pain worsens as the day progresses
-
Joint swelling after long periods of inactivity
-
Bone spurs and visible enlargement of affected joints
Rheumatoid Arthritis Symptoms:
-
Joint pain, stiffness, and inflammation
-
Redness and warmth around the affected joints
-
Morning stiffness lasting longer than one hour
-
Fatigue and general feeling of illness
-
Symmetrical joint involvement (both knees, for example)
-
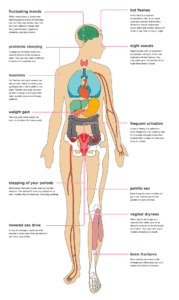
In severe cases, it can affect other organs such as the heart, lungs, and eyes
Joint Affected by OA and RA
OA generally affects joints that are subjected to repetitive use or injury, such as the knees, hips, hands, and spine. Since OA is a degenerative condition, it tends to worsen over time, and additional joints may become involved.
RA, on the other hand, can affect joints throughout the body. Commonly impacted joints include the wrists, ankles, feet, elbows, and knees. As an autoimmune disease, RA can also have systemic effects, impacting the heart, lungs, and other organs.
Risk Factors for OA and RA
Both OA and RA share some common risk factors, such as age and genetics. However, they also have their own unique set of risk factors.
Risk Factors for OA:
-
Age, particularly over 50
-
Joint injuries or overuse
-
Obesity
-
Family history of OA
-
Gender (more common in women, especially after menopause)
Risk Factors for RA:
-
Genetics and family history
-
Smoking and environmental exposures
-
Diet and lifestyle factors
-
Hormonal factors (more common in women)
-
Obesity
Causes of OA and RA
The exact causes of both OA and RA remain subjects of ongoing research. In OA, the primary cause is the breakdown of cartilage due to wear and tear over time, although joint injuries and repetitive use also contribute. For RA, the cause is less understood but is thought to involve a combination of genetic predisposition and environmental factors like smoking or infections.
Treatment Options for OA and RA
Both OA and RA require a multi-faceted approach to treatment, including medication, lifestyle changes, and sometimes surgery.
OA Treatment:
-
Pain relief through NSAIDs or over-the-counter medications
-
Physical therapy to improve joint function
-
Weight management to reduce joint stress
-
In severe cases, surgery such as joint replacement
RA Treatment:
-
Disease-modifying antirheumatic drugs (DMARDs)
-
Biologics to target specific immune system components
-
Steroids for inflammation
-
Pain relief through NSAIDs
-
Surgery to correct joint damage in advanced stages
Conclusion: Understanding the Differences Between OA and RA
Although both osteoarthritis and rheumatoid arthritis are forms of arthritis, they have distinct causes, symptoms, and treatment options. Understanding these differences can help in early diagnosis and better management of the conditions. If you experience any symptoms related to OA or RA, it’s important to consult with a healthcare professional for an accurate diagnosis and appropriate treatment plan.
Frequently Asked Questions
Which is Worse—Rheumatoid Arthritis or Osteoarthritis?
This question varies depending on the severity of each individual case. Generally, RA can be more debilitating due to its autoimmune nature and potential to affect multiple organs. However, OA can also significantly impact mobility and quality of life.
Can Osteoarthritis Be Mistaken for Rheumatoid Arthritis?
Yes, due to overlapping symptoms like joint pain and stiffness, OA can sometimes be misdiagnosed as RA. However, a proper medical evaluation and tests like X-rays can help distinguish between the two.
Can an X-Ray Differentiate Between Osteoarthritis and Rheumatoid Arthritis?
Yes, an X-ray can reveal the degree of joint damage, such as cartilage loss in OA or joint lining damage in RA. However, further tests like blood work or joint fluid analysis are often needed for a conclusive diagnosis.
Key Takeaways
-
OA and RA have distinct causes, symptoms, and treatments.
-
OA is more common with age and involves cartilage breakdown, while RA is an autoimmune disease.
-
Both conditions require early diagnosis and appropriate treatment to manage symptoms effectively.