Ocular Hypertension_ Everything to Know About Lowering Eye Pressure
Understanding Ocular Hypertension: What You Should Know About Elevated Eye Pressure
Estimated Reading Time: 7 minutes
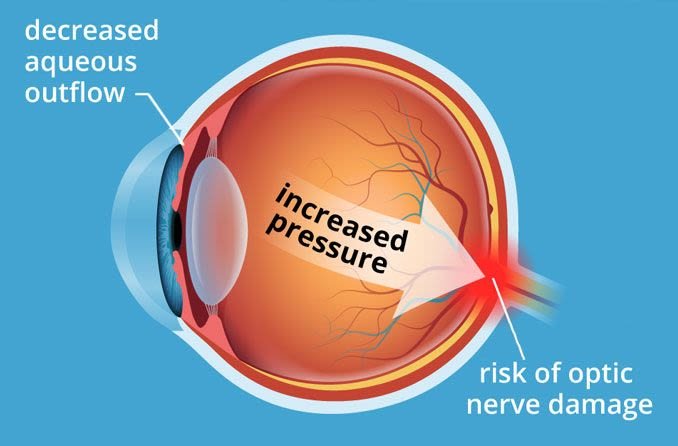
Ocular hypertension refers to increased pressure inside the eye, known as intraocular pressure (IOP), which occurs when fluid within the eye doesn’t drain properly. While it doesn’t typically cause noticeable symptoms or vision changes, untreated ocular hypertension can eventually damage the optic nerve—the critical link between the eye and brain—and increase the risk of developing glaucoma.
What Causes Ocular Hypertension?
Several conditions can interfere with fluid drainage from the eye, resulting in elevated IOP. These include:
-
Pigment Dispersion Syndrome: Pigment granules from the iris flake off and block the eye’s drainage system, particularly the trabecular meshwork.
-
Pseudoexfoliation Syndrome: Protein fibers accumulate near the drainage angle, restricting fluid outflow.
-
Uveitis: Inflammation in the eye’s middle layer can raise eye pressure.
-
Cataracts: Clouded lenses may obstruct fluid from exiting the eye.
-
Eye Tumors: Growths can physically block the drainage angle.
-
Steroid Medications: Long-term use of corticosteroids may increase IOP.
-
Surgical or Traumatic Eye Changes: Injuries or previous surgeries may alter the eye’s anatomy, leading to higher pressure.
-
Narrow Angles: Naturally narrow drainage pathways can result in fluid buildup.
Risk Factors for Developing Ocular Hypertension
You’re more likely to experience ocular hypertension if you:
-
Are over the age of 40
-
Are extremely nearsighted or farsighted
-
Have diabetes or high blood pressure
-
Are of African American or Hispanic descent
-
Take steroid medications or Topamax (topiramate)
-
Receive frequent eye injections
-
Have a family history of glaucoma or ocular hypertension
-
Have been diagnosed with pigment dispersion or pseudoexfoliation syndrome
Normal vs Elevated Eye Pressure
Typical eye pressure ranges from 10 to 20 mm Hg. Ocular hypertension is usually diagnosed when IOP exceeds 21 mm Hg. Pressures below 10 mm Hg are considered low (hypotony) and may also cause concern if they drop below 5 mm Hg.
Link Between Ocular Hypertension and Glaucoma
Not all individuals with ocular hypertension develop glaucoma, but elevated pressure increases the risk. The optic nerve’s tolerance to pressure varies by person. This is why regular monitoring is essential, especially because ocular hypertension often has no warning signs.
Why Ocular Hypertension Is Often Overlooked
Because the condition is usually symptom-free, people often believe their eyes are healthy until vision loss occurs from glaucoma. This highlights the importance of early detection and consistent monitoring.
How Eye Pressure Is Measured
Routine eye exams are the first step in identifying ocular hypertension. Eye doctors use a test called tonometry to measure IOP. Methods include:
-
Applanation Tonometry: After numbing the eye, a small device gently touches the surface to measure pressure.
-
Non-contact Tonometry (air puff test): Uses a quick burst of air to check pressure.
-
Rebound Tonometry (iCare) and TonoPen: Portable tools often used in screenings.
Treatment Options for Lowering Eye Pressure
Reducing IOP can help prevent damage to the optic nerve. Eye drops are the first line of treatment and work in two main ways:
1. Improving Fluid Drainage
-
Prostaglandin Analogs: Help fluid drain more easily (e.g., Xalatan, Travatan Z, Lumigan).
-
Rho Kinase Inhibitors: Relax the drainage channels (e.g., Rhopressa).
-
Cholinergic Agents: Constrict the pupil to enhance drainage (e.g., Isopto Carpine).
-
Nitric Oxide Donors: Relax the trabecular meshwork (e.g., Vyzulta).
2. Reducing Fluid Production
-
Beta-Blockers: Decrease fluid production (e.g., Timoptic, Betoptic).
-
Carbonic Anhydrase Inhibitors: Lower fluid output (e.g., Azopt, Trusopt). Diamox is the oral version, often used in urgent situations.
-
Alpha-Adrenergic Agonists: Both reduce fluid production and increase drainage (e.g., Alphagan P, Qoliana).
Potential Complications of Ocular Hypertension
If left unmanaged, ocular hypertension can lead to glaucoma, damaging the optic nerve and causing permanent vision loss. A serious complication is angle-closure glaucoma, where fluid drainage is suddenly blocked, requiring emergency care.
Symptoms of Acute Angle-Closure Glaucoma May Include:
-
Intense eye pain
-
Blurred vision or halos around lights
-
Nausea or vomiting
-
Sudden vision loss
Seek immediate medical help if you experience these symptoms.
Is Ocular Hypertension Reversible?
While ocular hypertension can be managed, it cannot be cured. Medications effectively reduce IOP and lower the risk of glaucoma by more than 50%. However, the condition needs ongoing treatment and monitoring.
When to See an Eye Doctor
If you’ve been diagnosed with ocular hypertension, follow your eye doctor’s schedule for checkups—even if you aren’t on treatment yet. Any discomfort or visual disturbances should be reported right away, as they could signal a progression to glaucoma.
Final Thoughts
Ocular hypertension often goes unnoticed, but it’s a serious risk factor for glaucoma and vision loss. With regular eye exams and proper management, most people can control their eye pressure and maintain healthy vision. Don’t wait for symptoms—get your eyes checked regularly to catch any changes early.
💬 Frequently Asked Question: Can Eye Pressure Be Reversed?
Although you can’t cure ocular hypertension, managing it with the right medication and routine eye exams can significantly reduce your risk of glaucoma and long-term damage.
⭐ Pro Tips for Managing Eye Health
-
Take your prescribed eye drops exactly as directed.
-
Share your medication list with your eye doctor, especially if you’re using steroids.
-
Avoid rubbing your eyes or self-treating eye discomfort without medical guidance.
-
Stick to regular eye exams—even if you feel fine.
✅ Key Takeaways
-
Ocular hypertension increases your risk of glaucoma but often has no symptoms.
-
Early detection through regular eye exams is crucial.
-
Medications can effectively reduce intraocular pressure and protect vision.
-
Management is ongoing—there’s no permanent cure.
📣 Stay Informed
Want more health insights like this? Subscribe to our newsletter for expert tips and updates on eye care and overall wellness!